This leaflet answers common questions about having a portacath inserted and how to care for it afterwards. If you would like further information, or have any worries, please do not hesitate to ask your nurse or doctor.
In all cases, a doctor will explain the portacath insertion procedure to you and answer any questions you may have.
In most cases, it will be possible for a friend or relative to accompany you for all, or part, of the procedure. Please ask your nurse or doctor.

What is a portacath?
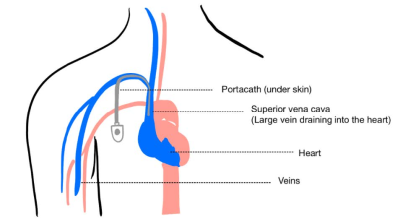
A portacath is a hollow flexible plastic tube which is placed into a large vein leading into the heart. It is generally used to give fluids, treatment medications like chemotherapy, or blood transfusion. It can also be used to take blood samples. A portacath is designed to stay in your body for as long as the treatment lasts, which can be up to several months or years.
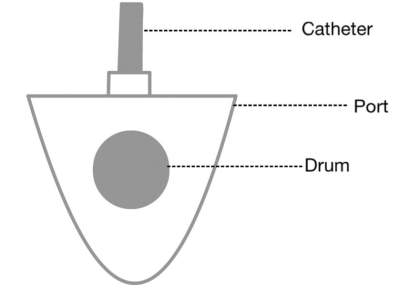
A portacath consists of two parts:
- The port: this is a small plastic chamber with a rubber drum in the middle, which is implanted underneath the skin of your upper chest. A special needle is inserted through your skin and into the rubber drum to provide treatment or to take bloods.
- The catheter: this is a hollow flexible plastic tube with its tip placed at the entrance to the heart. The other end is connected to the port.
How is a portacath inserted?
The insertion of a portacath is performed by an interventional radiologist. They are a doctor that specialises in using imaging for diagnosis, to perform procedures and to administer treatment. Local anaesthesia numbs the area we are working in which enables you to be awake during the procedure.
A small cut is made in the lower neck to pass the catheter into the vein leading into the bigger veins of your chest. A larger cut is made on your upper chest wall to insert the port. We will then close the cuts usually with dissolvable stitches and glue.
You will have two dressings, one on the port site and one at the base of your neck. This will result in two small permanent scars. A small visible bump will also be seen over where the port is inserted.
Before your procedure
Prior to coming in, a radiology nurse will carry out a pre-procedure assessment, usually by telephone. They will arrange for you to have some necessary blood tests, which may be able to be done at your local hospital if you prefer.
Please have a list of prescribed medicines ready for them to review. If you have any allergies, please be sure to mention them. You must also tell us if you have previously had a reaction to intravenous contrast medium, which is the dye used for certain x-rays and CT scans.
If you are on any medication which thins the blood (for example, aspirin, clopidogrel, warfarin, rivaroxaban, apixaban etc), please let your doctor or nurse know as we may need to stop them temporarily before the procedure. The number of days you will need to stop taking them depends on the type of medication you are on.
Do not eat anything from midnight on the day of the procedure. You may continue to drink water and take your medicines as prescribed, unless otherwise directed.
You will be asked to change into a theatre gown and may need to have a cannula put into your arm so that we can give you medication before, during or after the procedure. The interventional radiologist will discuss the procedure with you and will ask you to sign a consent form. You have the right to withdraw your consent to the procedure at any stage, by telling a member of staff.
Some patients have the procedure under sedation, but please note that this is not suitable for everyone.
Sedation
Sedation can be offered but it may not be suitable for everyone. This can be discussed further when you come in for the procedure.
Will insertion be painful?
Before we start, will give you a local anaesthetic injection, which numbs the area we are working on. It will sting for a few seconds before making the area completely numb.
During the procedure
The procedure typically takes around one hour. You will then be observed for four to six hours after the procedure before you are allowed to go home.
After your procedure
Most people have their portacath inserted as a day case using local anaesthetic. You will be allowed to go home around four to six hours after the procedure has been completed.
Risks and side-effects
Inserting a portacath is a safe procedure performed by experienced interventional radiologists. However, no procedure is risk-free. As we are putting a needle into your vein, there is a risk of bleeding, but this would usually be a small amount. Although we perform the procedure in a sterile environment, there is also a small risk of infection in the days or weeks after the procedure.
Once the local anaesthetic wears off, you may have some bruising and tenderness around the site of the port. This is normal and should only last for a few days. You may take some simple painkillers such as paracetamol.
Alternatives to a portacath
Your oncology team, with your input, have decided that a portacath is the best procedure for you. Alternatives would include a PICC (peripherally inserted central venous catheter), which is a long plastic tube that is inserted into an upper arm vein.
Care of the portacath
Dissolvable stitches and glue are usually used to close the port site. Glue and steri-strips may be used to close the neck scar. Although the glue is resistant to water, it is not fully waterproof, so it is recommended to keep the area dry for seven to ten days after the procedure. The glue will fall off by itself within a week- there is no need to peel it off. The steri-strips will also come off naturally - please do not peel them off. Once the scars have healed, it is safe to have baths, showers and to go swimming.
The dressings can be removed 48 hours after the procedure. When treatment is administered, the portacath is accessed using a special needle, which is secured in place using a water-resistant dressing. It will then be flushed after any treatment to keep it open.
The portacath should be flushed at least once a month to prevent blockages. Flushing can happen in the hospital or in the community by district nurses. Specific arrangements can be made by talking to your treating team.
What should I look out for?
Please contact your clinical team immediately, including out of hours, if you experience any of the following:
- redness
- swelling of neck or arm
- shortness of breath
- discharge from the scars (blood or pus)
- fever over 38C
- chills
How long after insertion can the portacath be used?
It can be used immediately but it is generally scheduled to be inserted a few days before your first treatment is due. If you have a gripper needle inserted into the port, you must not shower or bath until after the needle is removed. A gripper needle is a needle which is inserted into the port, with a plastic tube attached to it to allow easy access each time you need treatment.
Removal of portacath
The portacath is removed when it is no longer needed, and your treatment is complete. It may also be removed before your treatment is finished if you develop an infection in the area. This is carried out by the surgical team.
Driving after the procedure
If you have had sedation, you should not drive for 24 hours. It is advised that you do not drive for at least 48 hours after the port has been placed to allow healing.
Return to work
You can return to work, but you should avoid heavy lifting or strenuous tasks for at least one week.
Exercise
It is advised that you do not do any strenuous activities for at least one week. Avoid any weightlifting or carrying heavy objects as this could cause the port stitches to come undone Carrying a child may also cause the port stitches to come undone.
 Translate
Translate