News list
-

Could you be a Royal Free London governor?
Date published: 2 July 2025
News Categories:
-
Governors
-
-

Share your views on children’s surgery proposals
Date published: 23 June 2025
News Categories:
-
Trust news
-
Patient news
-
-

New role empowering cancer CNSs
Date published: 20 June 2025
News Categories:
-
Staff
-
Trust news
-
-

Staff awarded for excellence in education
Date published: 18 June 2025
News Categories:
-
Staff
-
Awards
-
Teaching
-
Trust news
-
-
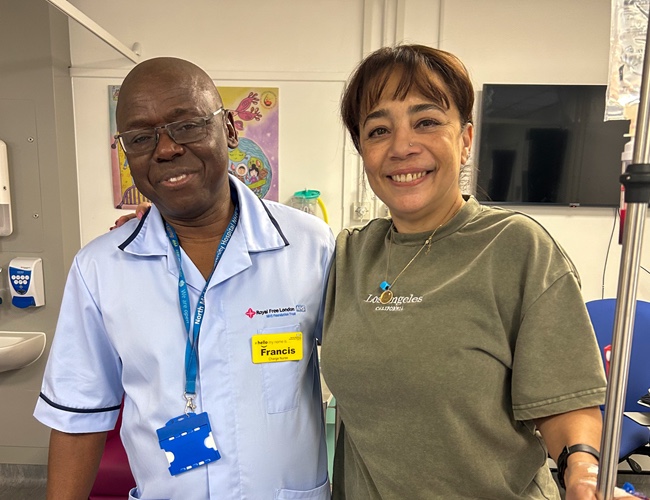
“Blood donations gave me my life back”: North Mid patient urges the public to donate this National Blood Week
Date published: 13 June 2025
News Categories:
-
North Middlesex University Hospital
-
Patient news
-
-

North Middlesex University Hospital hosts National Blood Week event with Spurs legend Ledley King
Date published: 11 June 2025
News Categories:
-
North Middlesex University Hospital
-
-
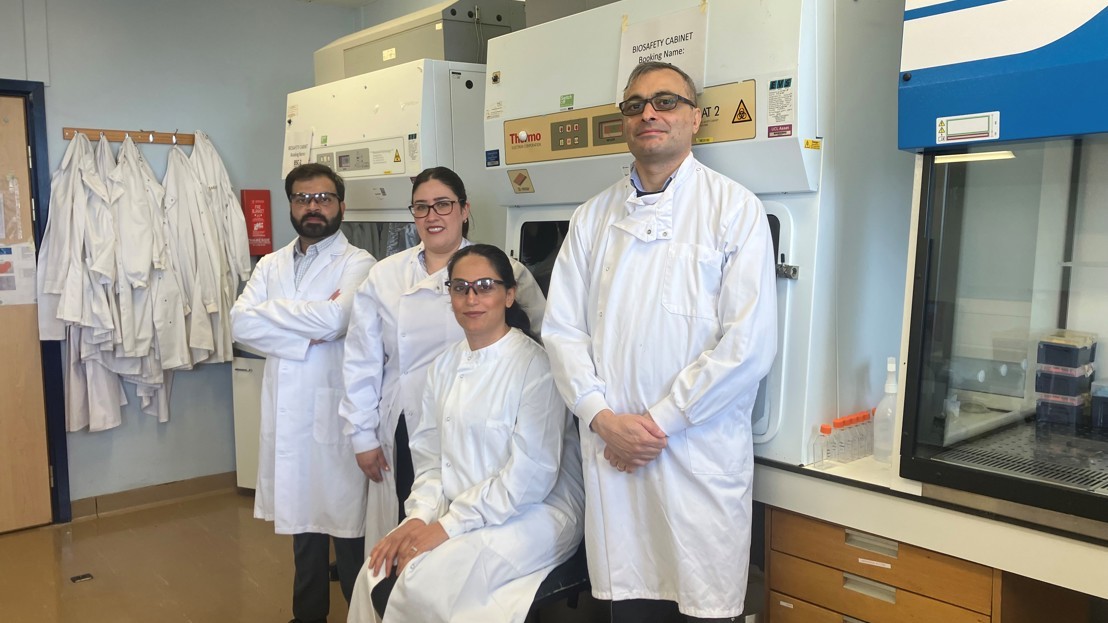
Human sample service plays crucial role in research
Date published: 11 June 2025
News Categories:
-
Research
-
-

Greener MRI scanner set to widen research opportunities at the RFL
Date published: 10 June 2025
News Categories:
-
Research
-
Royal Free Hospital
-
-

Celebrating one year of championing population health
Date published: 4 June 2025
News Categories:
-
Trust news
-
-

Groundbreaking breast screening study at Royal Free London
Date published: 3 June 2025
News Categories:
-
Research
-
Viewing 10 of 1806 results
 Translate
Translate