 A team of radiologists and chest physicians who introduced a new and more efficient lung biopsy method at Barnet Hospital (BH) have been shortlisted for an NHS innovation award.
A team of radiologists and chest physicians who introduced a new and more efficient lung biopsy method at Barnet Hospital (BH) have been shortlisted for an NHS innovation award.
The team’s innovative ambulatory lung biopsy service enables the vast majority of patients to be discharged just 30 minutes after the biopsy. The method also allows biopsy patients who suffer a collapsed lung to be treated at home as out-patients.
In most hospitals throughout the NHS and the rest of the world, patients who undergo even routine lung biopsies are admitted to hospital and remain in a hospital bed for four to six hours in order to monitor for lung collapse (pneumothorax).
However, patients that experience pneumothorax at Barnet Hospital are treated with a small, compact device called the Heimlich valve chest drain (HVCD), instead of a traditional bulky chest drain. The portable device allows those patients to leave hospital almost immediately and treat their collapsed lung safely and effectively at home.
Researchers suggest the new method, which has never been used in Europe before, could free up hundreds of hospital beds while also allowing more patients to undergo diagnostic biopsy in a much shorter space of time, leading to earlier lung cancer diagnoses. The new method also allows clinicians to biopsy patients who would usually not be eligible for the procedure due to the high risk of lung collapse.
While most hospitals of equivalent size to Barnet Hospital expect to do around 40 biopsies each year, thanks to the new method BH expects to have performed around 300 between April 2015 and April 2016. Currently, BH is the only European hospital using the early discharge/out-patient HVCD method. However, NHS England is now looking into how it could be adopted by hospitals across the capital and the rest of the UK.
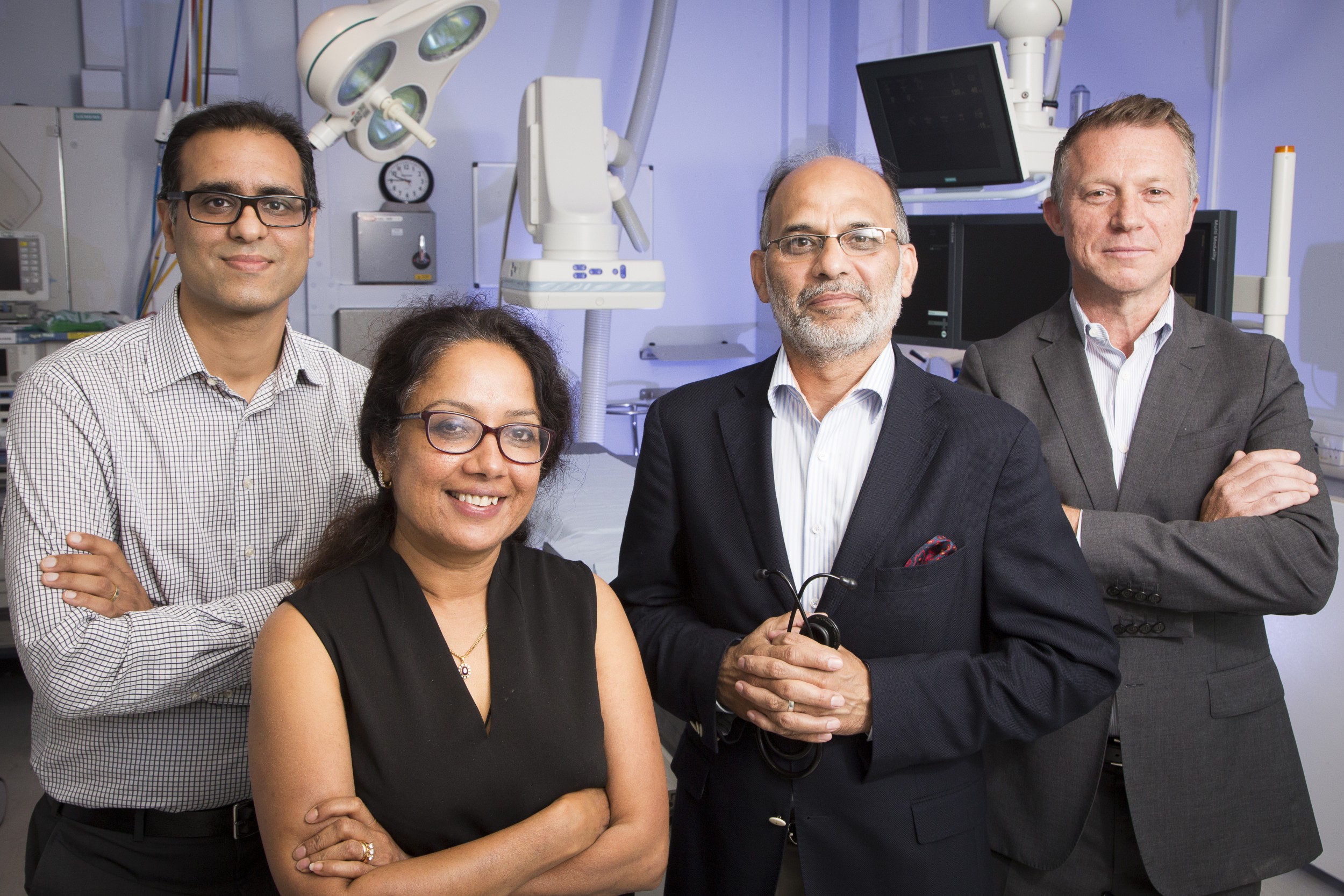
The team, which is led by Dr Sam Hare, consultant thoracic radiologist and radiology lead, has now been shortlisted for an NHS Innovation Challenge Prize in the ‘cancer care’ category.
The prizes seek to encourage, recognise and reward front line innovation and drive adoption of these innovations across the NHS. The team will be asked to present the lung biopsy project to a team of judges later this month.
Dr Hare said: “It is a tremendous honour for our work to be recognised by the shortlisting panel. Our overwhelming feeling is that driving adoption of this innovation across the NHS will be a game changer for the UK lung cancer landscape by providing earlier diagnosis in more patients. We are driven to do our utmost to win the award so that the current ‘Barnet Hospital model’ can shape a better future for lung cancer patients throughout the NHS.”
Image: (L-R) Dr Sam Hare, Dr Rama Vancheeswaran, Dr Sajid Khan, Dr Dean Creer
Ends
Notes to editors
Media contacts: daniel.obrien1@nhs.net or call 020 7317 7740.
About the Royal Free London NHS Foundation Trust
The Royal Free began as a pioneering organisation and continues to play a leading role in the care of patients. Our mission is to provide world class expertise and local care. In the 21st century, the Royal Free London continues to lead improvements in healthcare.
The Royal Free London attracts patients from across the country and beyond to its specialist services in liver and kidney transplantation, haemophilia, renal care, HIV, infectious diseases, plastic surgery, immunology, Parkinson's disease, vascular surgery, cardiology, amyloidosis and scleroderma and we are a member of the academic health science partnership UCLPartners.
In July 2014 Barnet Hospital and Chase Farm Hospital became part of the Royal Free London. Read 'A bigger trust, a better future'.
 Translate
Translate