A new machine which mimics the human body and allows doctors to store donor livers for an additional 24 hours could help more patients receive a life-saving organ transplant.
The Royal Free Hospital (RFH) is the first trust in London to use the device and has already carried out several successful transplants aided by the machine.
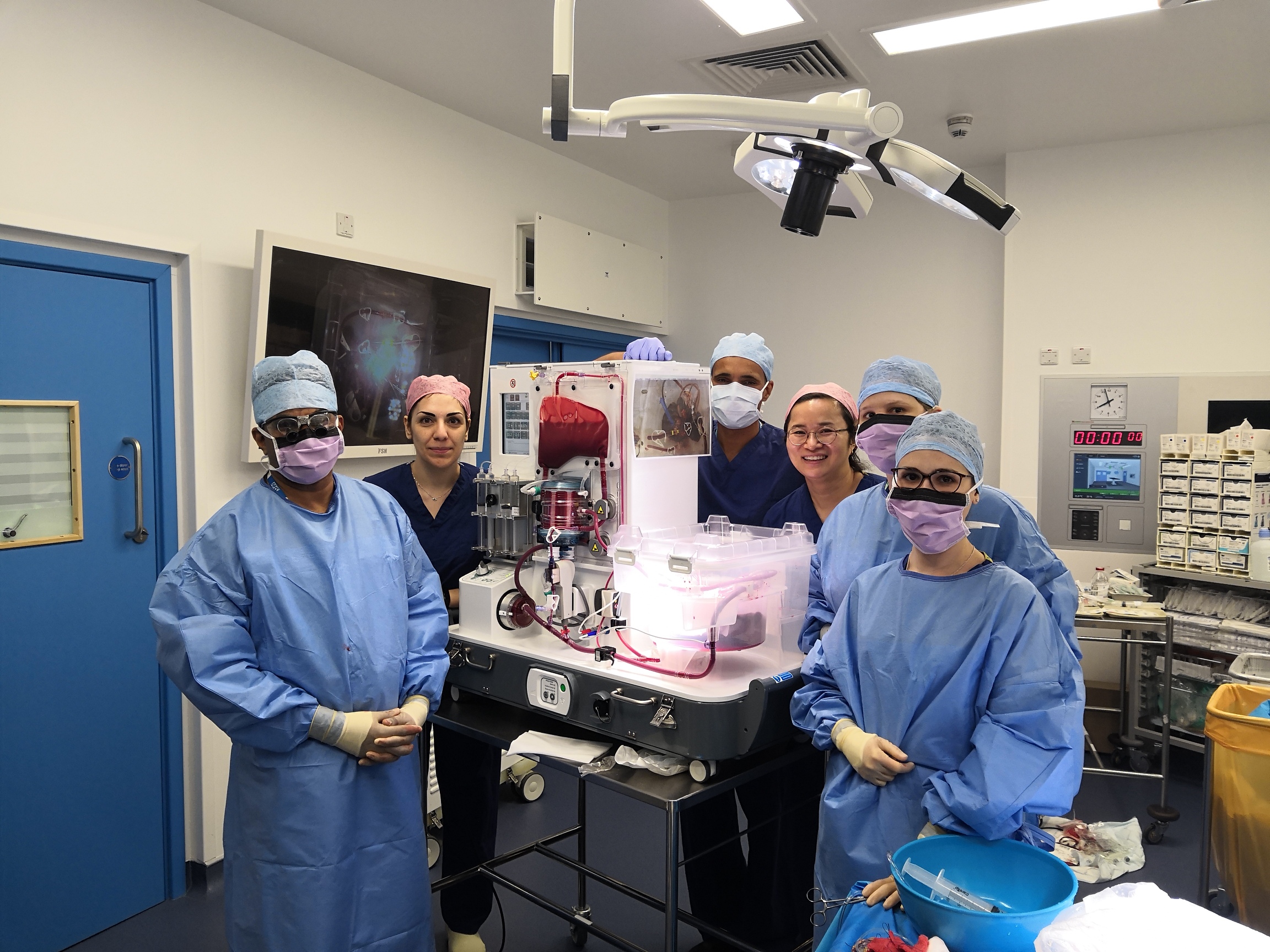
Rather than keeping livers on ice as is traditional, doctors at the RFH now have the option to use the OrganOx metra, a device which mimics the human body by keeping donor livers at body temperature and pumping oxygenated blood, medications and nutrients into them, to preserve the donated organ.
The metra allows doctors to assess how well the donated liver functions, which means they have a better understanding of whether it is suitable for transplantation.
It means that patients such as former NHS chef Trevor Williams are more likely to have a successful transplant.
Trevor, from Waterlooville, Hampshire, was the first NHS patient to receive a liver transplant using the metra at the RFH.
The 69-year-old was diagnosed with inoperable liver cancer in November 2018 and the only treatment option was a liver transplant.
Trevor first came in for the procedure in March but it was cancelled at the last minute after the liver was deemed unsuitable.
A week later he was matched with a new donor liver, which was first assessed on the OrganOx device and this time the transplant went ahead and was a success.
Satheesh Iype, the consultant surgeon at the Royal Free Hospital who carried out Trevor’s transplant, said: “In trials, the OrganOx device showed superior results to the regular method of storage. It is appropriate to use in cases where donor liver quality might be difficult to assess because it simulates the conditions in the body so you can assess its functionality before making a decision whether or not to transplant. This means that we can potentially accept more donor livers that before might not have been judged to be suitable and that means we are likely to perform many more transplants.”

L-R: Profesor Joerg-Matthias Pollok (clinical lead), Elaine Burrell (liver transplant co-ordinator), Trevor Williams, Lee Gutcher (operations manager for liver services) and Mr Satheesh Iype (surgeon).
Mr Williams added: “I didn’t hesitate to say yes when I was told about the possibility of harnessing this new technology for my transplant and it is incredible to think about it. The expertise and care I have received have been outstanding. From my consultant to the transplant co-ordinators, Mr Iype and the nursing staff. I can only say thank you. They and my donor have given me a new lease of life. I’m already planning a couple of trips to Great Yarmouth with my wife and we’ll also be going in our motor home to some steam rallies.”
In 2017, over 500 livers from deceased organ donors in the UK were either not retrieved or retrieved but not transplanted. In many cases this was because the donor organ was in a poor condition after being kept in an ice box.
The donor liver is attached to the machine for a minimum of four hours but can then remain there for up to 24 hours. Professor Joerg-Matthias Pollok, clinical lead for hepato-pancreato-biliary (HPB) surgery and liver transplantation at the RFH, was instrumental in bringing the OrganOx machine to the trust. He said: “Surgeons are conservative people who need to be convinced that something is really good for their patient. When you get offered a donor liver we make decisions on the information provided and sometimes we have to decline an offer based on that information. But this new technology has given us an objective way of assessing the liver because we can measure how it is performing.”
Doug Thorburn, clinical director for liver transplantation, HPB and hepatology, said: “The arrival of the OrganOx machine is great news for our patients, many of whom currently wait a long time to get a new liver. This is an important improvement in liver transplantation and we hope will lead to us to being able to perform more transplants at the Royal Free Hospital. As in all cases of organ donation we are so grateful to the donors and their families for giving their consent. It is the ultimate gift.”
 Translate
Translate