Staff at the Royal Free London are helping to launch the world’s first national tissue bank for pancreatic cancer, to push forward research into the cancer with the bleakest prognosis. 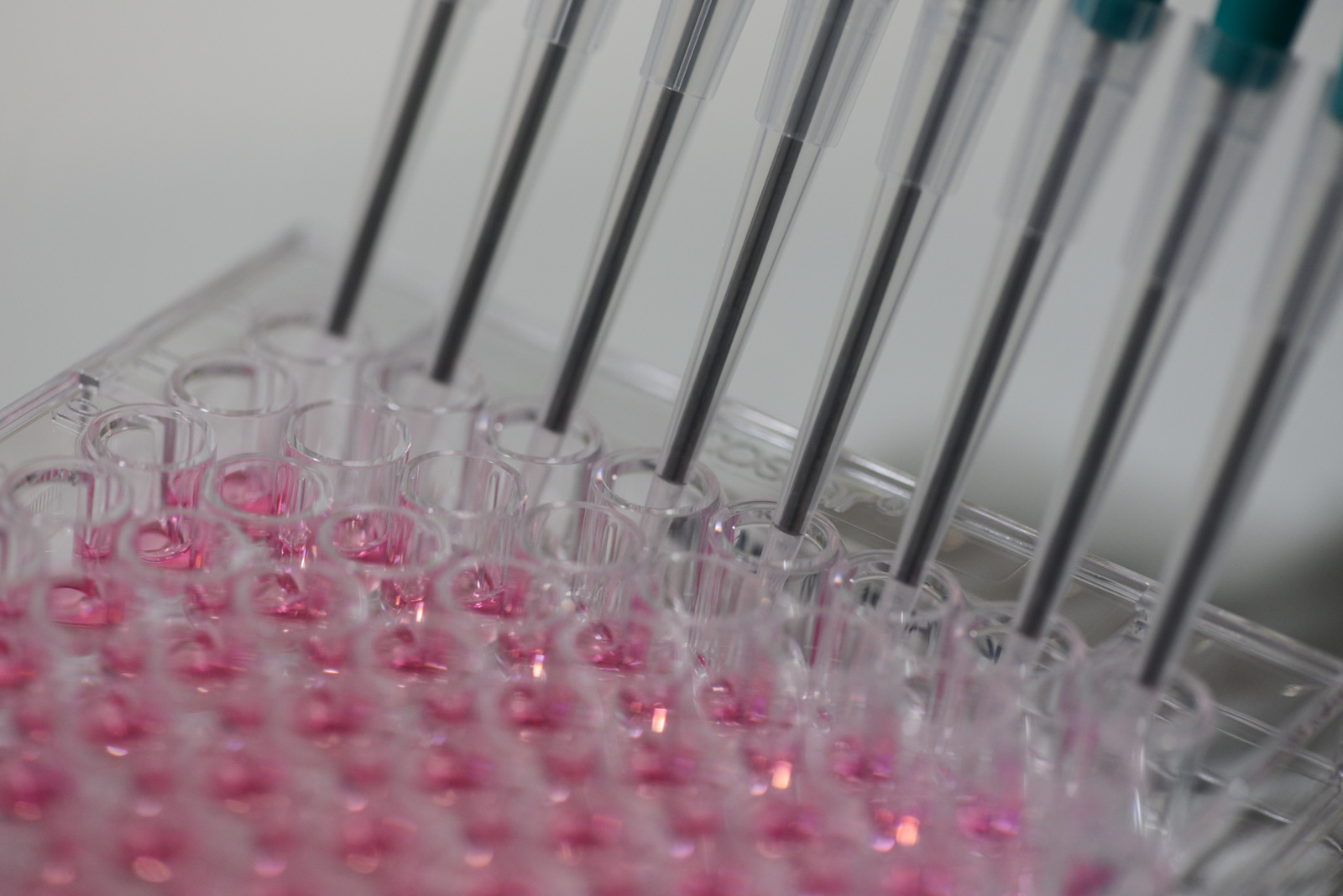
Samples from consenting patients from across the UK will be stored anonymously at the Pancreatic Cancer Research Fund Tissue Bank. They will be used by researchers to help them develop new treatments for pancreatic cancer, and to make those treatments available to patients sooner.
The Royal Free London is one of six key partners who will be collecting samples of tissues, blood, urine and saliva from 1,000 patients with pancreatic diseases each year. The samples will be stored in the main tissue bank at Bart’s Cancer Institute, Queen Mary University of London. The four other partners are ABM University Health Board in Swansea, University Hospitals of Leicester NHS Trust, Oxford University Hospitals NHS Foundation Trust and University Hospital Southampton NHS Foundation Trust.
The tissue bank is being funded with £2 million from the UK research charity, Pancreatic Cancer Research Fund (PCRF).
Maggie Blanks, chief executive of the tissue bank, said: “Researchers told us that progress was being held back by the scarcity of high-quality tissue samples on which they can test their ideas and validate their research. For research results to be more meaningful, the samples must be collected, handled and stored consistently, following strict procedures. A nationally co-ordinated tissue bank will not only ensure that more samples become available to researchers, but that these are quality controlled to provide a much better basis for the very best research to be carried out. It’s a huge commitment for the charity, but thanks to the generosity of our supporters we’ve been able to make it happen.”
 Professor Brian Davidson, who has been leading this project at the Royal Free Hospital, said: “This new tissue bank means that for the first time, researchers from all the country will have access to patient samples which have been stored following consistent procedures. This will allow more meaningful research to be carried out and will ultimately mean patients have access to better treatments sooner – this is a huge step forward.”
Professor Brian Davidson, who has been leading this project at the Royal Free Hospital, said: “This new tissue bank means that for the first time, researchers from all the country will have access to patient samples which have been stored following consistent procedures. This will allow more meaningful research to be carried out and will ultimately mean patients have access to better treatments sooner – this is a huge step forward.”
Around 8,800 people in the UK are diagnosed with pancreatic cancer each year. It is known as the UK’s deadliest cancer, with a survival rate of just 3% - a figure that has barely improved in 40 years. New treatments are desperately needed: surgery to remove the tumour offers the best chance of survival - but most patients are diagnosed when the cancer has already spread to other organs. Without surgery, the average survival time from diagnosis is six months.
The new facility, will store tissue donated by consenting patients with diseases of the pancreas undergoing biopsy or surgery. All samples will be anonymised before being banked.
Each donation will be logged with detailed medical and, where possible, genetic information so that researchers can request exactly the right type of sample for their research. Data generated by all research projects using tissue bank samples will be fed back into a bespoke database, and will be made freely available to the global research community, to inform and underpin their own research.
The development of the tissue bank has been driven by Professor Hemant Kocher, a pancreatic cancer researcher at Barts Cancer Institute and consultant pancreas and liver surgeon at the Royal London Hospital. He said: “This is a highly ambitious venture, but one that is crucial to enabling researchers to investigate new treatments for this most lethal cancer. At the moment, we can help only a small proportion of patients with surgery. For the majority of those diagnosed, and for those who see their cancer return even after surgery, there’s very little else we can offer.
“The tissue bank will also help us to tackle this disease with earlier diagnosis,” he added. “Many proteins associated with pancreatic cancer are also found in blood, urine and saliva, so having these materials from patients alongside the tissue samples helps us to find ways to diagnose the disease at an earlier, curative stage,” he added.
“We’re already in discussions with more hospitals around the UK who are interested in becoming partner centres. This underlines the determination of all those in the UK’s pancreatic cancer community to really pull together and drive progress.”
Ends
Bottom image: Professor Brian Davidson.
Notes to editors
Media contacts: mary.mcconnell2@nhs.net or call 020 7472 6665
All partner centres are licensed by the Human Tissue Authority and the Pancreatic Cancer Research Fund Tissue Bank has secured ethical approval from National Research Ethics Service.
While reserves are being built up, applications for samples will be invited from researchers at all the collaborating centres and those engaged in current and completed projects funded by PCRF. The tissue bank will be open to applications from any researcher in the UK from year three, and as stocks become sufficiently available, to international researchers.
About the Royal Free London NHS Foundation Trust
The Royal Free began as a pioneering organisation and continues to play a leading role in the care of patients. Our mission is to provide world class expertise and local care. In the 21st century, the Royal Free London continues to lead improvements in healthcare.
The Royal Free London attracts patients from across the country and beyond to its specialist services in liver and kidney transplantation, haemophilia, renal care, HIV, infectious diseases, plastic surgery, immunology, Parkinson's disease, vascular surgery, cardiology, amyloidosis and scleroderma and we are a member of the academic health science partnership UCLPartners.
In July 2014 Barnet Hospital and Chase Farm Hospital became part of the Royal Free London. Read 'A bigger trust, a better future'.
About Pancreatic Cancer Research Fund (PCRF)
PCRF is the only UK charity dedicated exclusively to funding research into pancreatic cancer.
To date, PCRF has funded 34 research projects worth some £5.2 million, covering a diverse range of approaches to tackling pancreatic cancer, including virotherapy, immunotherapy, new drug targets and biomarkers for early diagnosis as well as fundamental research to further the understanding of the disease at a molecular level.
 Translate
Translate