Our welcoming paediatric team provides a wide range of services for children in north London from birth to 18 years of age.
We have special wards, theatres, emergency departments and outpatient clinics tailored to children and young people to ensure they have the best experience possible when visiting us.
Paediatricians, neonatologists, nurses and allied health professionals — who are specialists in children’s health — care for children at our four main hospitals: Barnet Hospital, Chase Farm Hospital, North Middlesex University Hospital and the Royal Free Hospital, as well as providing outpatient clinics at Edgware Community Hospital.
Visit the NHS healthier together website for more advice for parents and carers of young children.
Helpful videos
Advice for parents or carers of children aged 0 to five.
Barnet Hospital and Chase Farm Hospital
To change or cancel a children’s clinic appointment:
Tel: 020 7443 9757 (for dermatology, ear, nose and throat, ophthalmology and maxillofacial)Tel: 020 7794 0500 ext 32312 (for all other clinic appointments)
Lines are open Monday to Friday, 9am to 5pm (excluding bank holidays).
North Middlesex University Hospital
Children's outpatient reception
Tel: 020 8887 2579
Email: northmid.
Paediatric day assessment unit
Tel: 020 8887 3095
Rainbow ward
Tel: 020 8887 2335 or 020 8887 4304
Paediatric assessment unit
Tel: 020 8887 3766
Enfield 0-19 service
Tel: 020 3988 7300
Email: northmid.
Royal Free Hospital
To change or cancel a children’s clinic appointment:
Tel: 020 7830 2144
Edgware Community Hospital
To change or cancel a children’s clinic appointment:
Tel: 020 3758 2420
- Please see our individual service pages for other contact information.
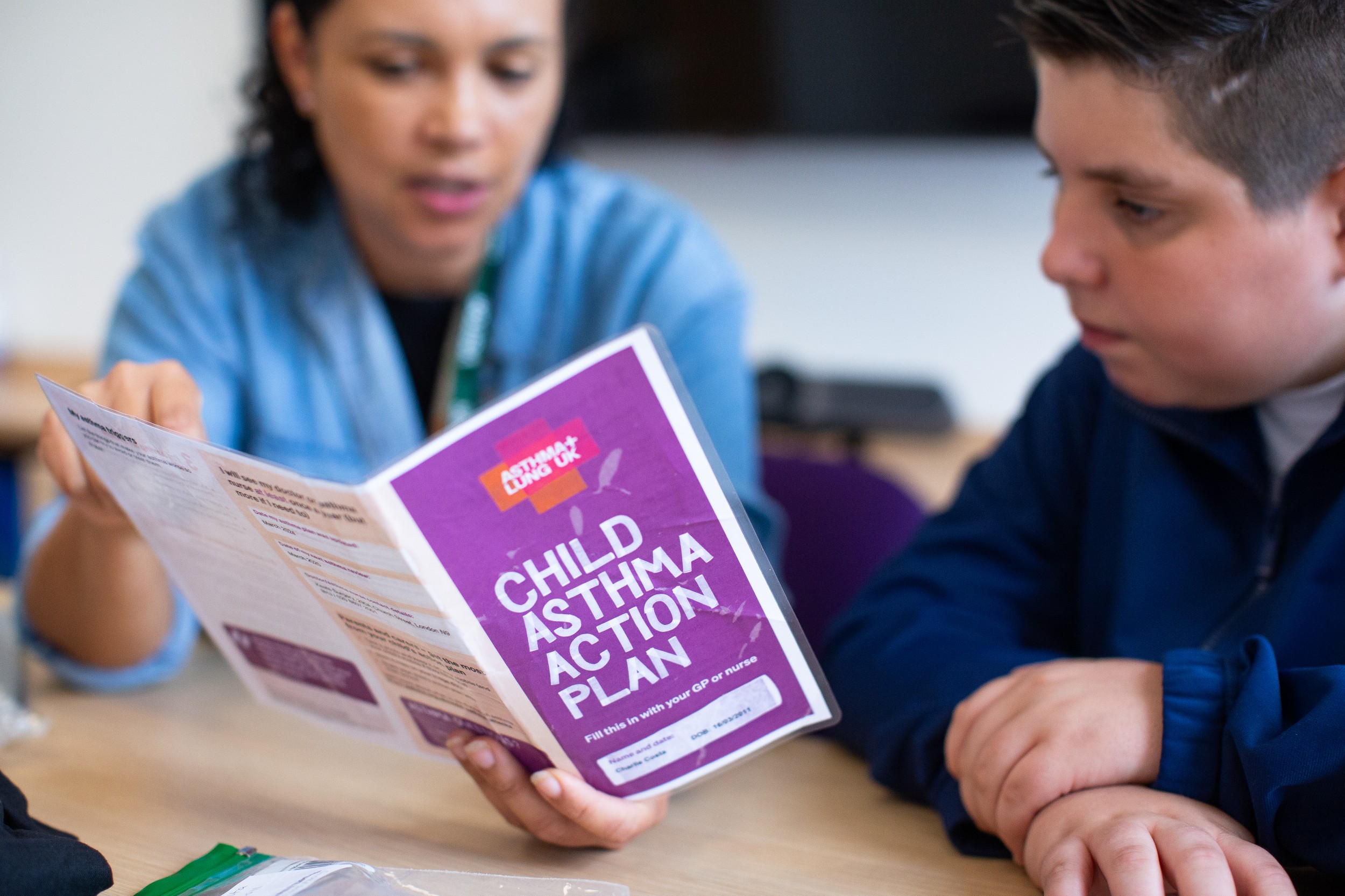
We run a wide range of specialist outpatient children’s clinics where children can visit us for their treatment and go home from hospital the same day.
What to bring with you
Please bring your appointment letter with you, along with your child's red book and any medication they are currently taking in original containers.
You are more than welcome to bring siblings with you to the appointment, however, please be aware that waiting room space is limited and you may be with us for some time, so they may become bored and unsettled.
If you do not attend your appointment and we do not hear from you, we will not routinely offer another appointment at the paediatric clinic and your child may be discharged back to the care of the referring doctor.
If you need to cancel or change your appointment at the children’s clinic, please call us during office hours on the contact numbers above.
Please get in touch and tell us if any of your contact or GP details change.
If you or your child is unwell
If your child is unwell on the day of the appointment, please let us know on the numbers above.
Norovirus, also known as ‘winter vomiting disease’, is highly contagious. It affects people of all ages and can be spread very easily through water, food, air and contact. Symptoms include vomiting, projectile vomiting, diarrhoea and raised temperatures.
If you or your child have experienced any of these symptoms in the past 48 hours, please do not visit the hospital.
If a child needs to be admitted to one of our hospitals, we have children’s wards at:
- Barnet Hospital: Galaxy
- Royal Free Hospital: 6 North
These wards have specialist medical staff including paediatric nurses to look after our young patients.
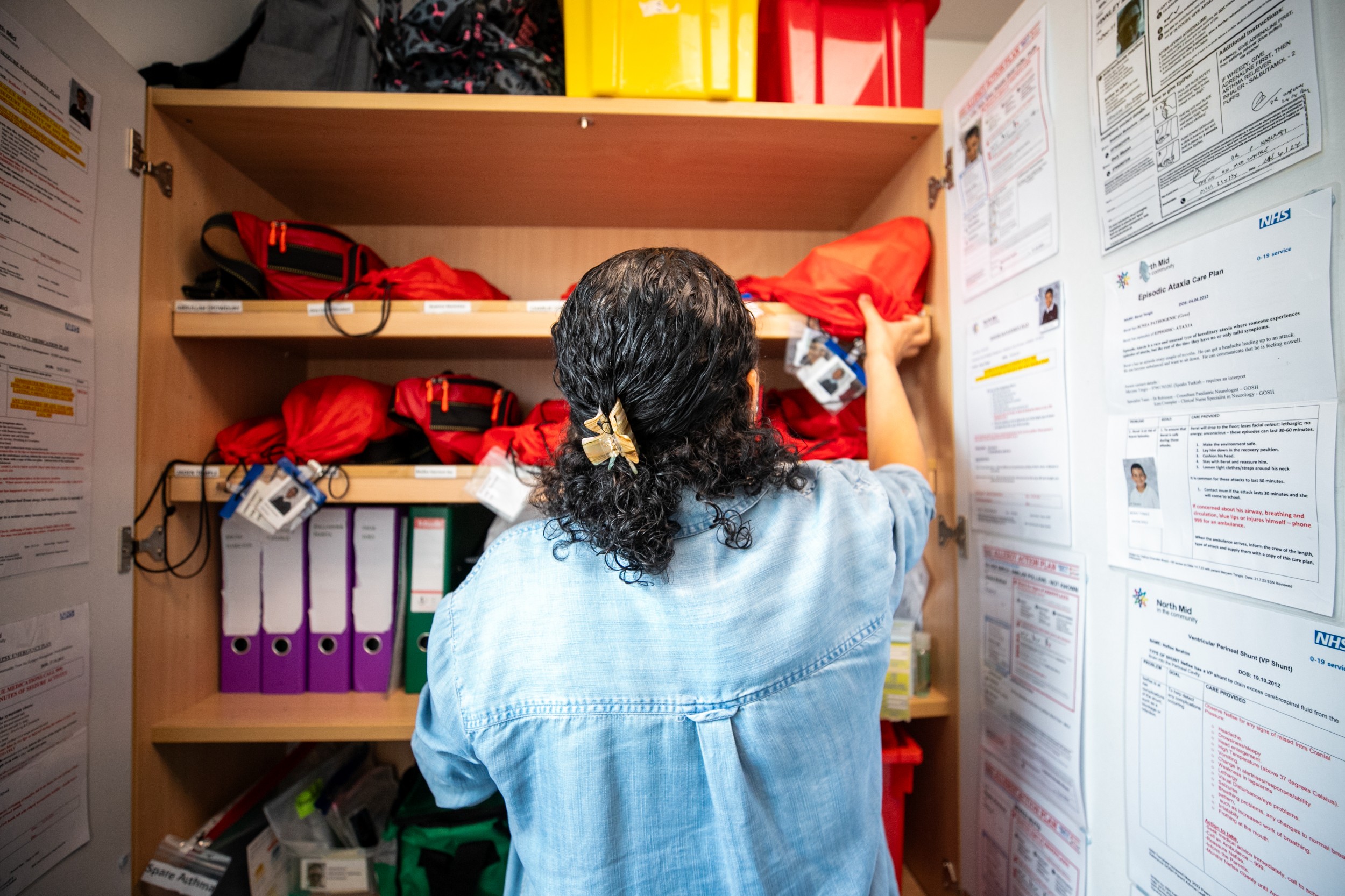
All members of staff wear a Royal Free London photographic identification badge.
Our nurses wear a navy-blue, child-friendly tunic and blue trousers, while other members of the team wear their own clothes.
Student nurses have placements on the wards, and they may be involved in caring for your child. All student nurses are supervised and only help look after patients suitable to their level of training.
We also have play teams at both these hospitals, who help children and young people feel at home and relaxed during their stay.
There is a well-equipped playroom with a team of play specialists, as well as a classroom staffed by teachers who will liaise with your child's school to provide hospital education. Televisions, DVDs, console games and toys are available, and staff organise other activities.
Our children’s wards have a combination of ward beds and side rooms (some with ensuite facilities), depending on clinical needs.
This is a day care ward for children and young people having surgical procedures or investigations that can be carried out in a day visit without the need to stay overnight.
At the Royal Free Hospital, it is at ward 6 North on the 6th floor of the hospital.
At Barnet Hospital, it is within the Galaxy children’s clinic which is next to Galaxy ward.
Play and education facilities are available for children, even if they are with us just for the day.
One parent or carer may stay overnight with their child.
We have beds or reclining chairs available for parents and there is a parents' rest room with a television and hot and cold drinks.
See our facilities for parents’ section on this page for more information.
There is open visiting for parents or carers on our children’s wards. All other family members are free to visit from 10am to 8pm (unless previously discussed with the paediatric nurse-in-charge).
Please keep visitors to a maximum of two people at any one time and ensure you watch over all children who are visiting with you to ensure a calm and relaxed environment for our young patients.
The doctors’ ward round usually starts at 10am and is repeated at intervals. Parents are welcome to attend to ask questions and meet your child, friend or relative’s medical team.
We offer a tempting menu of dishes to encourage children to eat and provide halal and kosher meals for children who require them. Parents can also bring meals and warm them up using hospital kitchen facilities.
Meals are served at the following times:
- Breakfast: 7.30 to 8.30am
- Lunch: 12.30pm
- Dinner: 6pm
Children do not need to miss out on their schooling while they are in hospital.
If your child is between the ages of five and 16 and they are well enough, he or she can attend the Royal Free Hospital Children's School next to the children’s ward at the Royal Free Hospital.
Children who are not well enough to visit the classroom can have bedside sessions.
For more information, visit the Royal Free Hospital Children's School website.
We know having a child in hospital can be a difficult experience and we do our best to make your stay with us as easy as possible. Please see below for the facilities available to parents.
- one parent bed by the patient's bed
- parents’ room with free tea, coffee and hot chocolate
- separate parent’s toilet and shower on the wards and inside most of the side rooms
- breakfast provided following overnight stays
- breakfast, lunch and dinner provided for breastfeeding mothers
- emergency supplies of toiletries
- baby changing facilities
- information sheets
- ward information folder by every bed at Barnet Hospital and in the parents' sitting room at the Royal Free Hospital
- Parents’ sitting room with a microwave, kettle and fridge. Hot meals are available for parents who are staying with their babies. There is also a small play area available for siblings.
- At Barnet Hospital, there are 10 individual care rooms giving parents the opportunity to stay in the hospital with their infant 24 hours a day and improving the opportunity for family-centred, developmental care. Each room has its own bed and recliner armchairs allowing both parents to have skin to skin contact with their baby as much as possible, and a breast pump to allow the mother to express at their baby’s bedside.
- At the Royal Free Hospital, there are four beds available on ward 6 West B for parents to stay with their babies prior to them going home. This is usually for one to two nights. If there is space, we also encourage mothers to stay prior to this to help support breastfeeding.
We aim to provide a supportive and caring service for children and young people requiring surgery, whether as inpatients or in our day surgery departments.
We have close ties with Great Ormond Street Hospital (GOSH) and visiting paediatric surgeons from GOSH run regular clinics and carry out surgery.
Our team, which includes a paediatric physiotherapist and is supported by the radiology and physiotherapy departments, also provide surgical care across a wide range of specialties including:
- ear, nose and throat surgery, including adenoidectomy or tonsillectomy (removal of tonsils and/or adenoids) and grommets to treat glue ear
- plastic surgery, including removing extra fingers or toes and ear reconstruction
- orthopaedic surgery, including problems with gait (how you walk)
- ophthalmic surgery, including squint corrections
- neonatal tongue tie service (where the movement of the baby’s tongue is restricted)
Children who are having surgery must stop eating and drinking before their operation. This is important because if there is food or liquid in your child’s stomach during the anaesthetic, it could come up into the back of the throat and damage their lungs.
Children are more comfortable if they do not wait for longer than necessary without food and drink. Children having an afternoon operation who miss their breakfast may feel more unwell after their operation, so it is important to try and make sure that they eat this meal.
We give the following timings at your child’s pre-operative assessment depending on if we expect the operation to be in the morning or afternoon. Please be aware that this may change. You will be given final instructions when you are phoned by the nurse the day before surgery:
Children having surgery in the morning
- Have a normal dinner the night before.
- Miss breakfast in the morning.
- Have small amounts of water up to one hour before surgery.
- Breastfed babies can have a feed four hours before surgery.
- Babies on formula milk can have a feed six hours before surgery.
Children having surgery in the afternoon
- Have a light breakfast on the day of surgery, to be finished by 6.30am.
- Have small amounts of water up to one hour before surgery.
- Breastfed babies can have a feed four hours before surgery.
- Babies on formula milk can have a feed six hours before surgery
Your doctor or nurse may offer you and your child the opportunity to take part in research, but if you are interested in taking part but have not been approached, feel free to ask your healthcare team if there are any studies for which you may be eligible.
Alternatively, please email rf-tr.
You can also visit our research pages to find out more about the types of research the Royal Free London is involved in.
Please see our individual service pages for referral information.
Where to go when your child is ill or injured
When your child is ill or injured, it is difficult to decide if or when to call your child’s GP, NHS 111, or go to the emergency department (A&E).
For advice on what to do and where to go if your child shows certain signs or symptoms of illness, see this guidance from the NHS.
Noah's Ark Children's Hospice
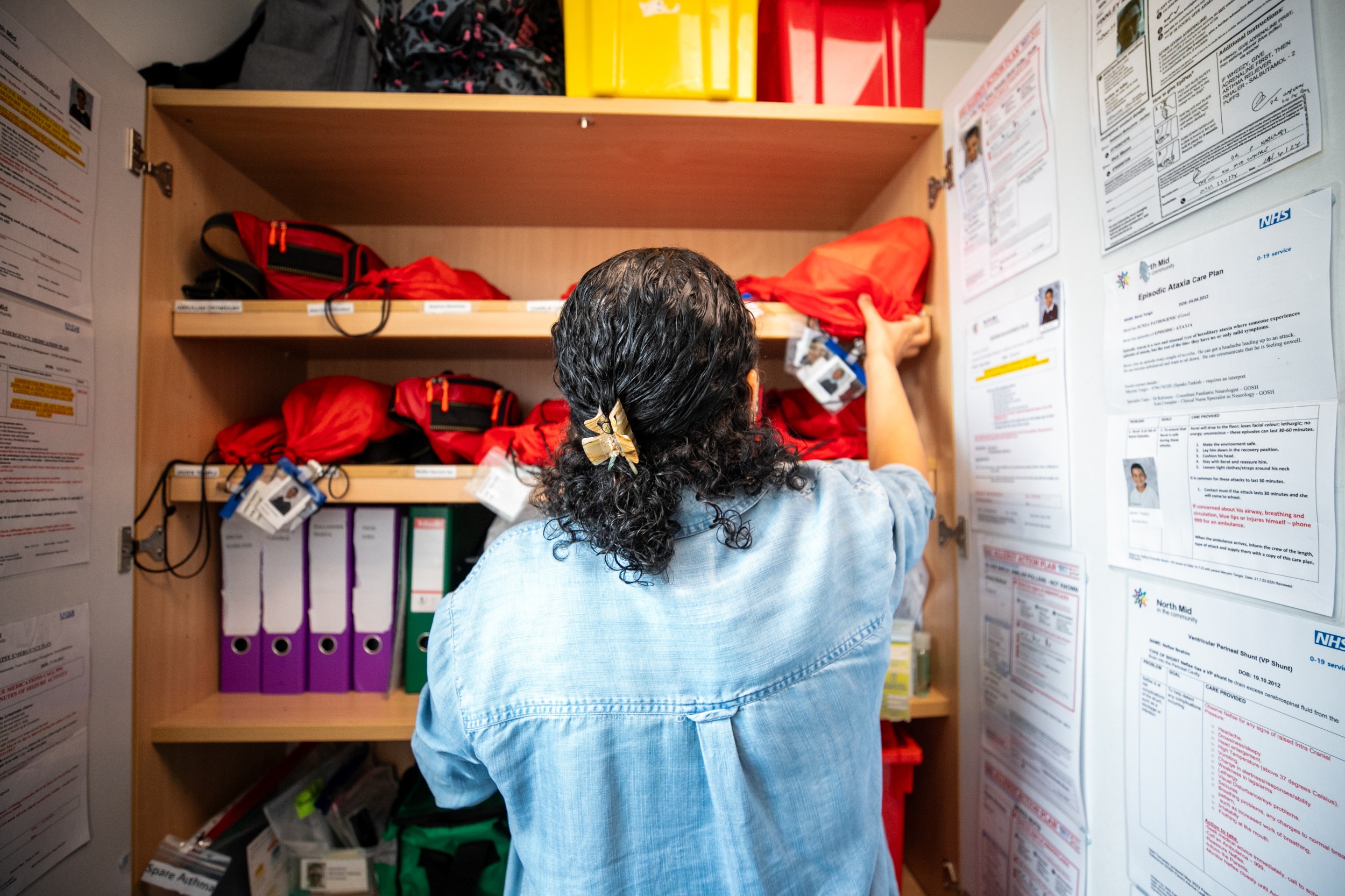
We are proud to be linked with Noah's Ark Children’s Hospice, which is in Barnet and provides clinical support and holistic care for children with life limiting and life-threatening conditions across north central London.
Children can be cared for in their home or in the hospice by expert nurses and specialist carers.
The whole family is supported by a variety of services and the care offered is bespoke for each child.
Useful websites
Listed below are websites that you may find useful when looking for further information, including advice for children needing help and phone numbers for social services and other helplines.
NSPCC
Childline: 0800 1111 (for under 18s)
NSPCC child protection helpline: 0808 800 5000
Talk to Frank
Drugs helpline: 0300 123 6600
SupportLine
Tel: 01708 765200
Email: info
Young Minds
Text SHOUT to 85258 (for young people)
Parents helpline: 0808 802 5544
Youth Access
Tel: 020 8772 9900
 Translate
Translate